Comprehensive Analysis of GLP-1 Medications Health Benefits, Weight Loss Efficacy, Side Effects, Safety, and Population Health Impacts
I thought this report was very helpful in showing the massive benefits GLP-1 medications and providing some metrics on side effects. Sources linked throughout.
The emergence of glucagon-like peptide-1 (GLP-1) receptor agonists represents one of the most significant advances in obesity and diabetes treatment in recent decades. Recent clinical trials demonstrate that these medications achieve unprecedented weight loss results, with Zepbound showing 47% greater relative weight loss compared to Wegovy in head-to-head studies ^2. Beyond weight management, comprehensive research reveals that GLP-1 medications impact 175 different health conditions, offering benefits ranging from cardiovascular protection to addiction reduction ^8. The rapid adoption of these therapies has coincided with concerning trends in American health, as obesity rates have reached 40.3% of adults and diabetes prevalence continues climbing to 11.6% of the population ^27.
Weight Loss Efficacy and Comparative Effectiveness
Superior Performance of Dual-Agonist Therapies
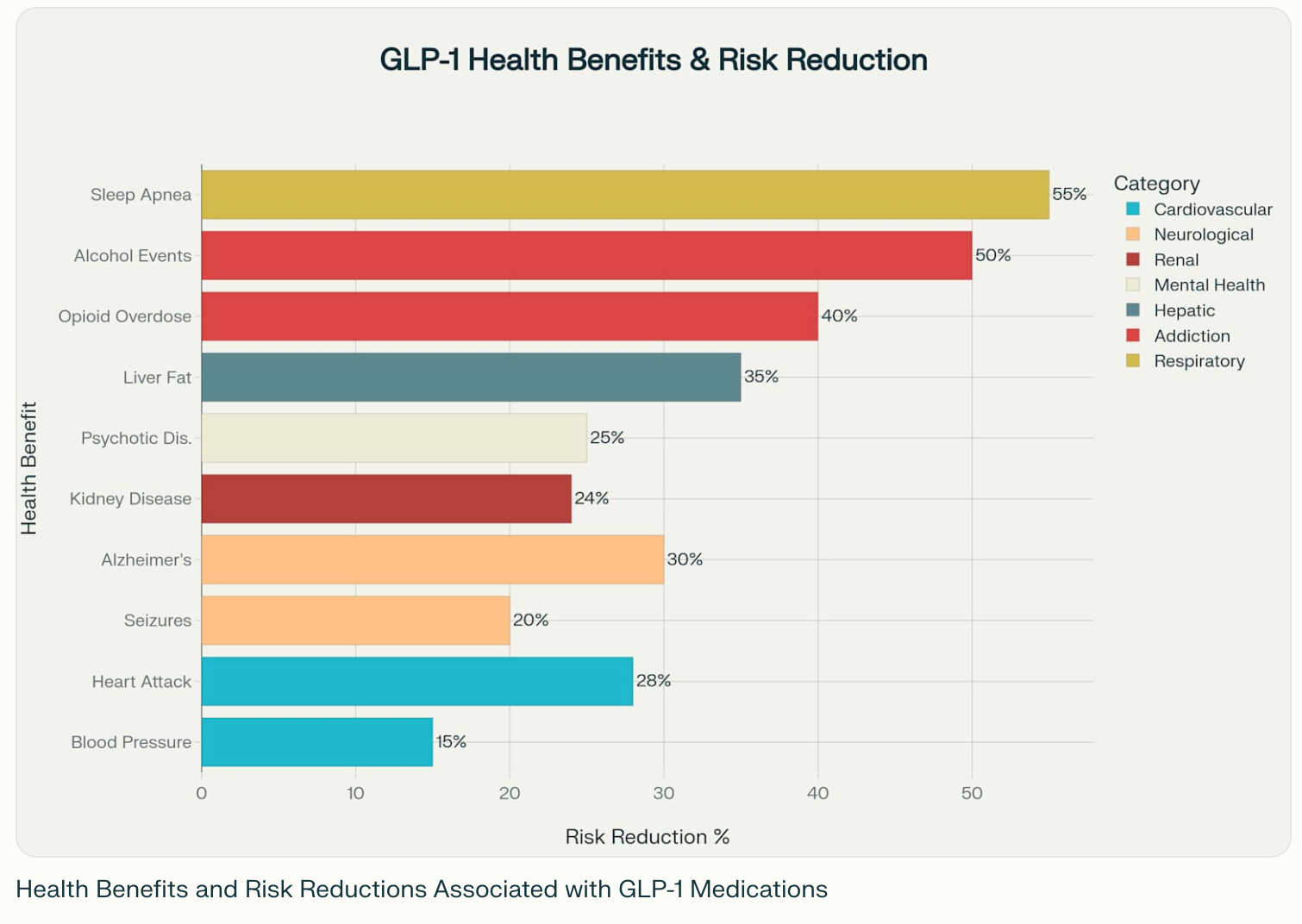
The SURMOUNT-5 head-to-head trial represents a landmark study comparing the two leading GLP-1 medications directly ^2. Participants using Zepbound (tirzepatide) achieved an average weight loss of 20.2% compared to 13.7% with Wegovy (semaglutide), translating to 50.3 pounds versus 33.1 pounds of weight reduction respectively ^2. This 47% greater relative weight loss demonstrates the enhanced efficacy of dual GIP and GLP-1 receptor agonism compared to mono GLP-1 receptor agonism ^5.
The most recent STEP UP trial data shows even more promising results with higher-dose semaglutide ^1. Participants receiving semaglutide 7.2 mg achieved 20.7% average weight reduction, with 33% of patients losing more than 25% of their body weight ^1. These findings suggest that dose optimization may significantly enhance treatment outcomes across the GLP-1 class ^1.
Average Weight Loss Percentage by GLP-1 Medication vs Placebo
Average Weight Loss Percentage by GLP-1 Medication vs Placebo
Sustained Weight Loss and Long-term Outcomes
Long-term efficacy data from the STEP 5 trial demonstrates the sustainability of weight loss with GLP-1 therapy ^3. After 104 weeks of treatment, 77% of patients maintained at least 5% weight loss, while approximately one-third achieved 20% or greater weight reduction ^3. The sustained nature of these results distinguishes GLP-1 medications from previous weight loss interventions, which typically show significant weight regain over time ^3.
Side Effects Profile and Safety Considerations
Common Gastrointestinal Effects
The safety profile of GLP-1 medications is predominantly characterized by gastrointestinal adverse events ^6. More than 75% of patients experience at least one side effect, with nausea, constipation, diarrhea, and vomiting being the most frequently reported ^2. These effects are generally mild to moderate in severity and tend to diminish over time as patients develop tolerance ^1.
Discontinuation rates due to adverse effects remain relatively low, with approximately 6% of Zepbound users and 8% of Wegovy users stopping treatment ^2. The overall GLP-1 class maintains a 5-10% discontinuation rate, which compares favorably to many other chronic disease medications ^6.
Serious Adverse Events and Monitoring Requirements
While rare, serious adverse events require careful monitoring and patient selection ^6. Pancreatitis occurs in 0.1-0.3% of patients, while gallbladder problems affect 0.2-0.5% of users ^6. Kidney-related complications, including nephrolithiasis and interstitial nephritis, have been reported in comprehensive safety analyses ^36. Healthcare providers must maintain vigilance for these complications, particularly in patients with pre-existing risk factors ^38.
Comprehensive Health Benefits Beyond Weight Loss
Cardiovascular Protection and Metabolic Improvements
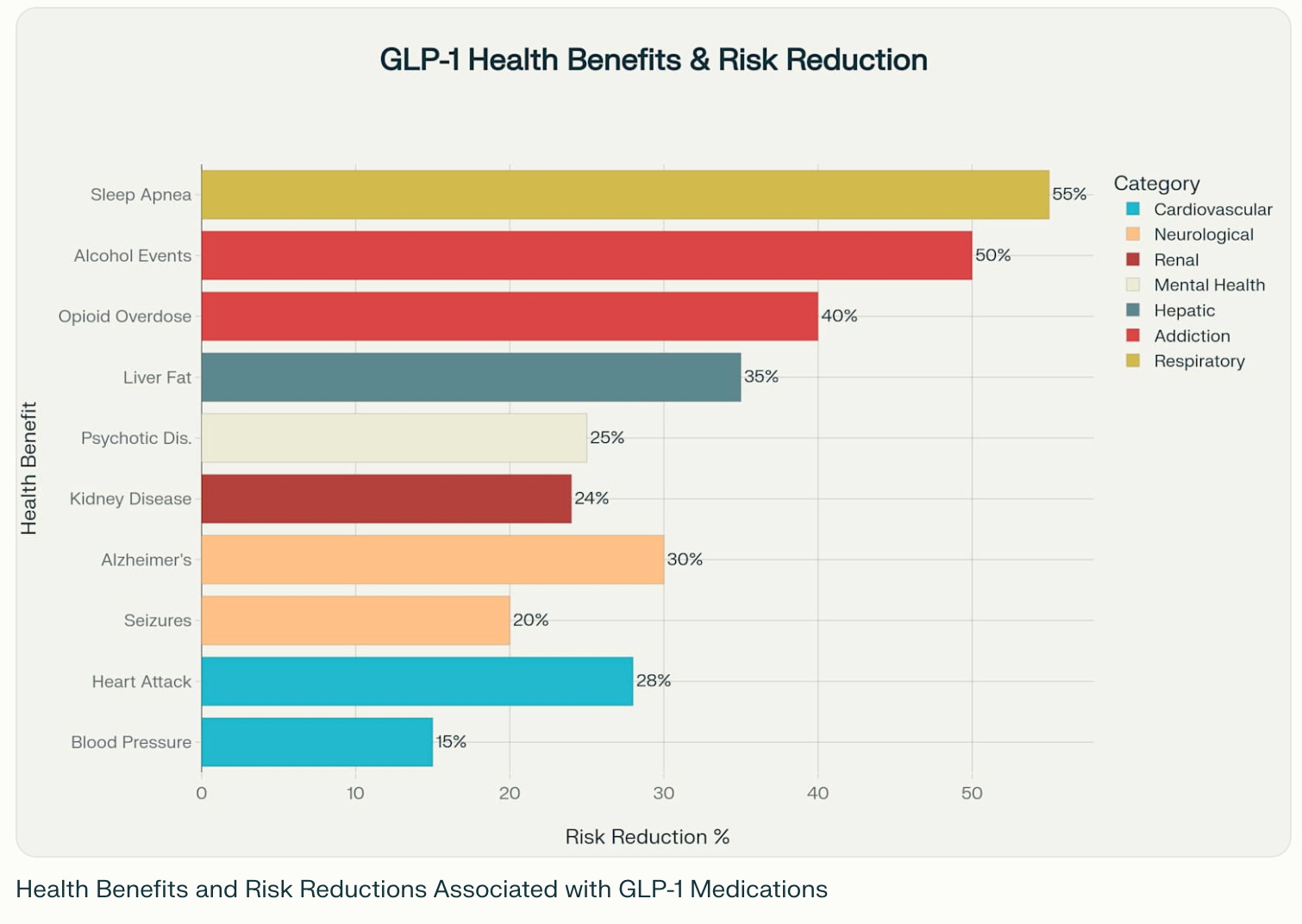
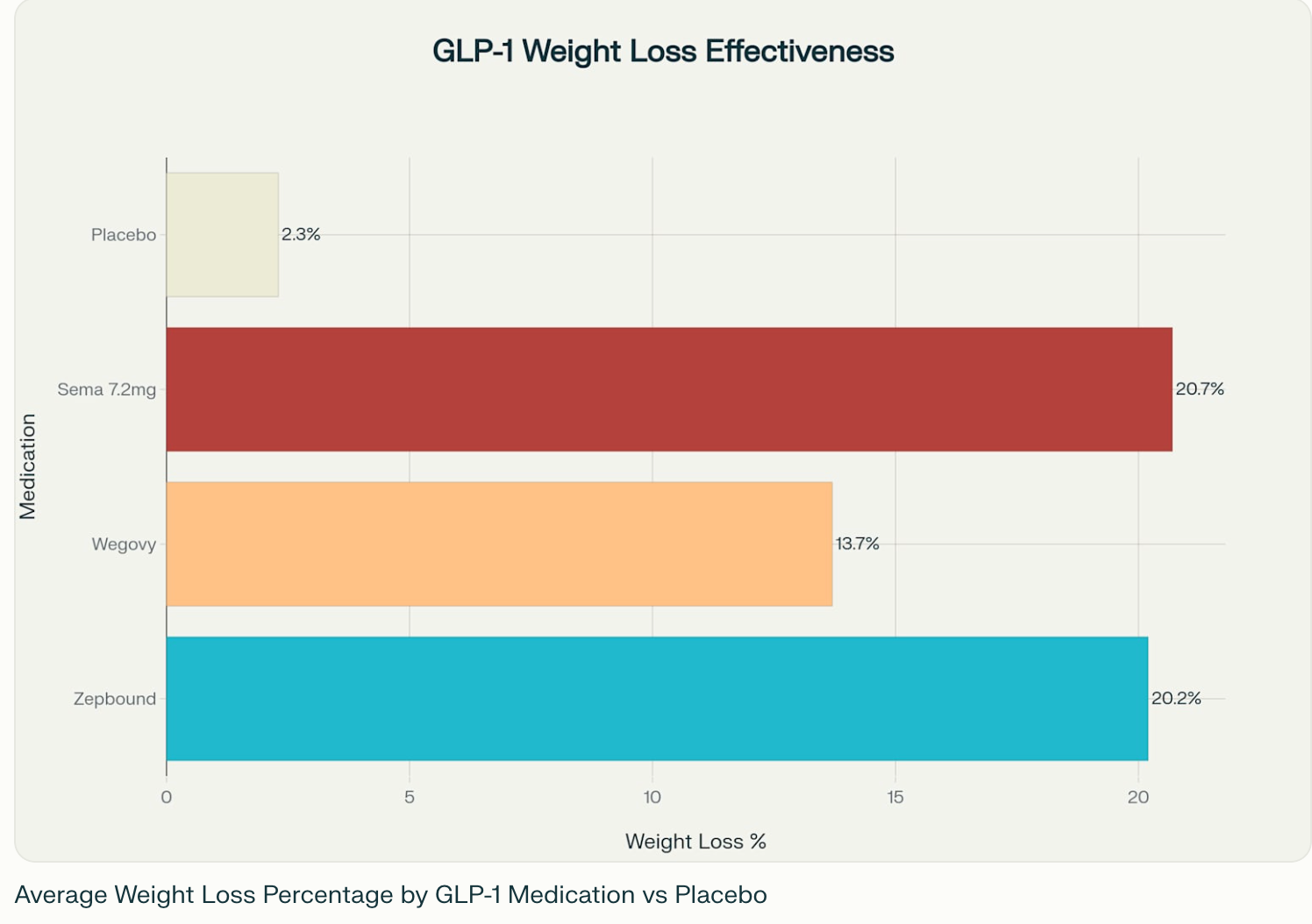
GLP-1 medications demonstrate significant cardiovascular benefits independent of their weight loss effects ^15. Meta-analysis of randomized controlled trials shows a 28% reduction in myocardial infarction risk and meaningful reductions in both systolic and diastolic blood pressure ^15. The SELECT trial established cardiovascular risk reduction as a class effect, leading to expanded indications for these medications ^1.
Addiction and Substance Use Disorder Benefits
Emerging research reveals remarkable effects on addiction-related behaviors ^9^11. Clinical trials demonstrate that semaglutide reduces alcohol consumption and craving in patients with alcohol use disorder ^9. Large-scale population studies show 50% lower rates of alcohol binging and 40% reduced opioid overdose risk among GLP-1 users ^16. These effects appear to result from the medications' impact on dopamine pathways and reward-seeking behavior ^10.
Sleep Apnea and Respiratory Improvements
Recent clinical trials demonstrate significant improvements in obstructive sleep apnea among GLP-1 users ^14. Patients receiving tirzepatide showed 55% improvement in sleep apnea symptoms compared to 5% improvement with placebo ^17. When combined with CPAP therapy, patients experienced 62.8% reduction in irregular breathing patterns ^17. These benefits likely result from both weight loss and direct effects on airway inflammation ^36.
Neurological and Cognitive Benefits
Comprehensive population-based studies reveal protective effects against neurodegenerative diseases ^8^38. GLP-1 use is associated with reduced risk of Alzheimer's disease, dementia, and seizures ^8. The medications appear to reduce neuroinflammation and may influence brain dopamine levels, contributing to these neuroprotective effects ^8.
Health Benefits and Risk Reductions Associated with GLP-1 Medications
Health Benefits and Risk Reductions Associated with GLP-1 Medications
Kidney and Liver Health Improvements
The FLOW trial demonstrated 24% reduction in major kidney disease events among patients with type 2 diabetes and chronic kidney disease ^39. Even in non-diabetic patients with chronic kidney disease, semaglutide reduces albuminuria by 52.1%, indicating significant renal protection ^43. For liver health, GLP-1 medications improve hepatic fat accumulation and liver enzyme levels, showing promise for non-alcoholic fatty liver disease treatment ^40.
Adoption and Usage Patterns in the United States
Rapid Growth in Prescription Rates
GLP-1 medication usage has experienced explosive growth in the United States ^18^22. The percentage of adults with GLP-1 prescriptions increased from 0.87% in 2019 to 4.03% in 2024, representing nearly 600% growth over six years ^18. This translates to approximately 12% of adults reporting ever using these medications, with 6% currently taking them ^19.
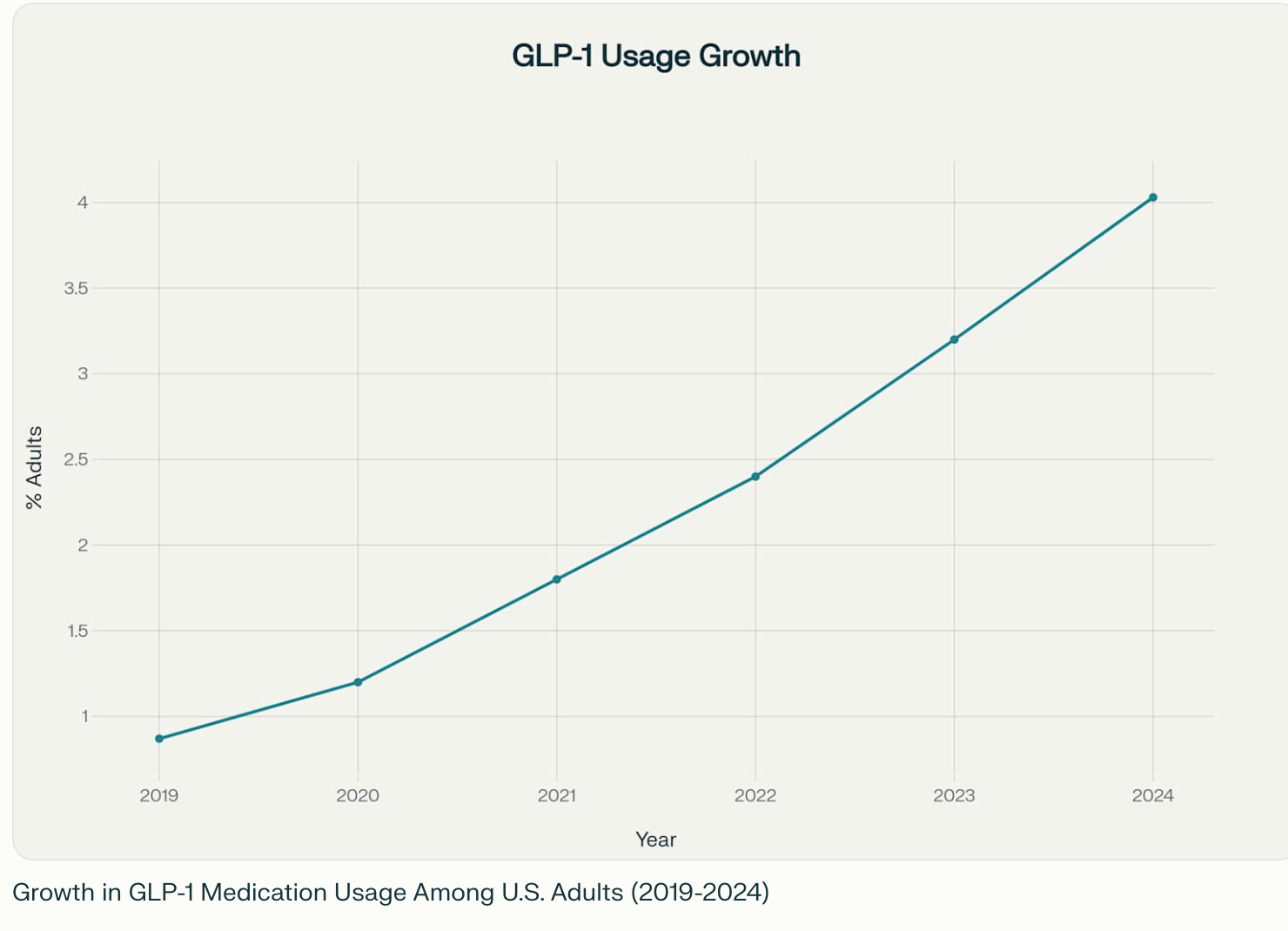
Growth in GLP-1 Medication Usage Among U.S. Adults (2019-2024)
Growth in GLP-1 Medication Usage Among U.S. Adults (2019-2024)
Prescription Patterns and Healthcare Provider Trends
Advanced practice practitioners and primary care physicians increasingly prescribe these medications, with APPs' share rising from 25.3% to 40.6% between 2017 and 2024 ^22. Monthly prescription volumes reached 1.5 million by February 2024, accounting for 0.41% of all prescriptions dispensed in the United States ^22. Wegovy prescriptions reached 0.42 million monthly, while Zepbound achieved 0.25 million monthly prescriptions within its first year of availability ^22.
Economic Impact and Access Challenges
The financial burden of GLP-1 medications remains substantial, with average prescription costs exceeding $1,500 ^26. Despite insurance coverage for many patients, approximately 54% of users report difficulty affording the medications ^19. The economic impact extends beyond individual costs, with GLP-1 therapies driving 6.7% of total drug costs and representing about half of all drug spending increases in 2024 ^25.
Usage Demographics and Treatment Patterns
GLP-1 prescriptions for weight loss show fastest growth among younger generations, with highest usage rates among adults aged 18-44 ^20. Among individuals with diabetes, 43% report ever taking these medications, while 22% of those told they are overweight or obese have used them ^19. Medicare coverage limitations significantly impact usage patterns, with only 1% of adults over 65 using GLP-1 medications for weight loss compared to higher rates in younger populations ^19.
Obesity and Diabetes Trends in America
Current Obesity Prevalence and Geographic Distribution
The United States faces an unprecedented obesity crisis, with 40.3% of adults classified as obese during 2021-2023 ^27. Geographic disparities are stark, with 23 states reporting adult obesity rates of 35% or higher ^28. The Midwest and South demonstrate the highest regional prevalence at 36.0% and 34.7% respectively ^29.
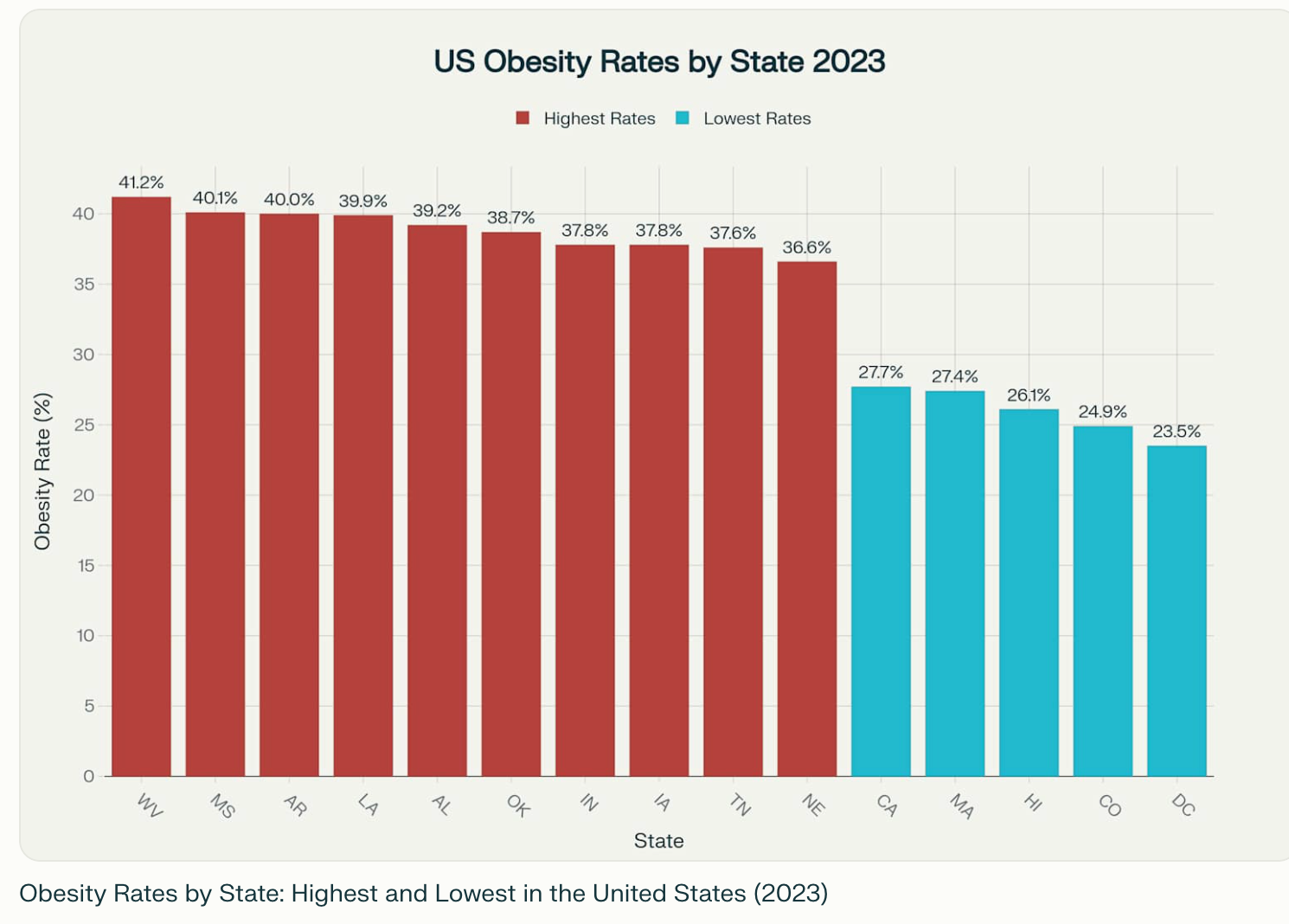
Obesity Rates by State: Highest and Lowest in the United States (2023)
Obesity Rates by State: Highest and Lowest in the United States (2023)
Severe obesity continues increasing despite overall obesity rates stabilizing, rising from 7.7% to 9.4% of adults ^27. This trend toward more extreme obesity categories presents particular challenges for healthcare systems and emphasizes the need for effective interventions ^30.
Diabetes Epidemic and Rising Prevalence
Diabetes prevalence has reached alarming levels, affecting 38.4 million Americans or 11.6% of the population ^35. The economic burden totals $412.9 billion annually, including $306.6 billion in direct medical costs ^33. Type 2 diabetes rates among youth increased 62% following the COVID-19 pandemic, with particularly severe impacts on Black and Hispanic children ^31.
Diabetes Prevalence Trends in the United States (2015-2024)
Diabetes Prevalence Trends in the United States (2015-2024)
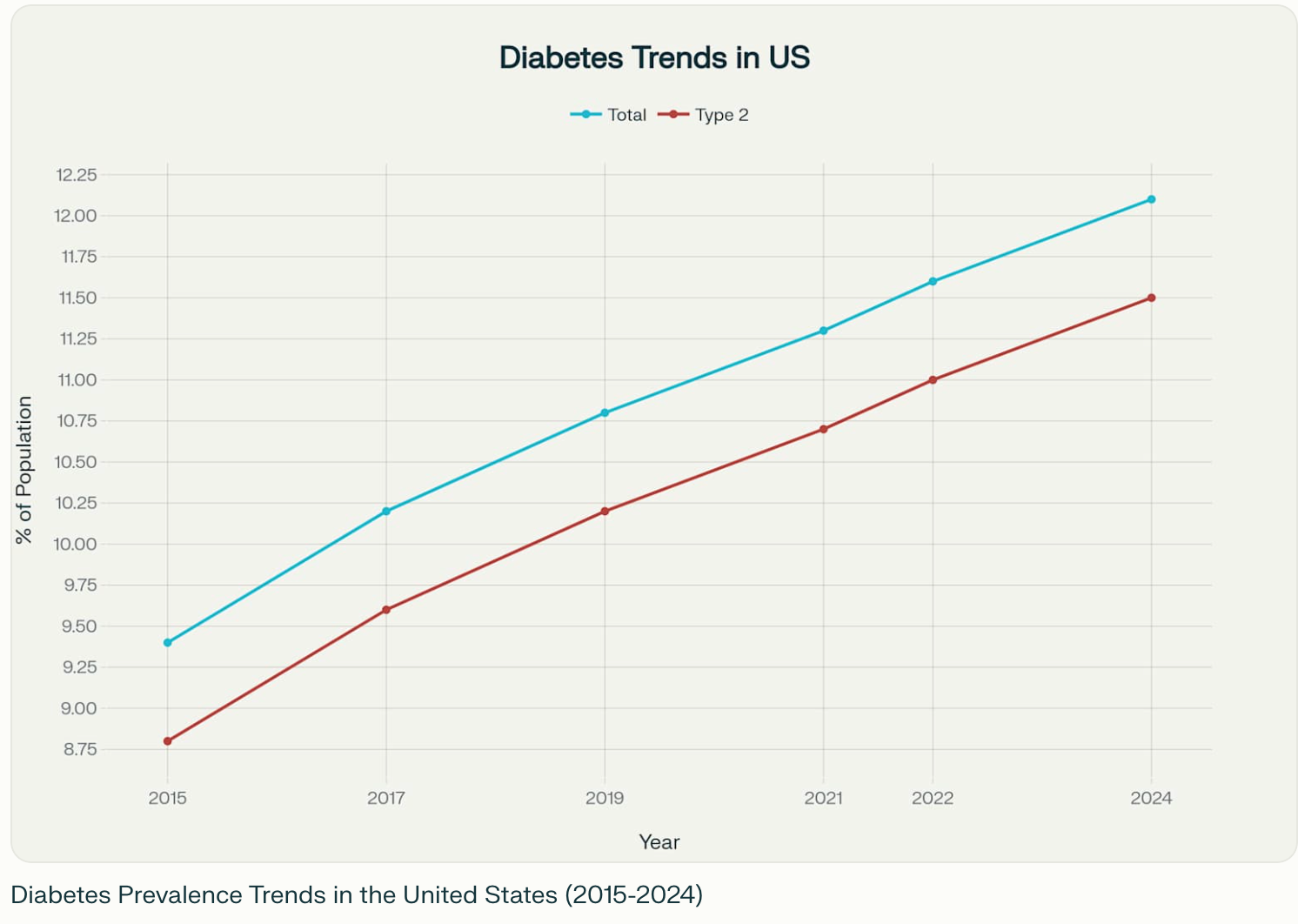
The prediabetes population encompasses 97.6 million Americans aged 18 and older, representing a vast reservoir of individuals at risk for developing diabetes ^35. Annual diabetes diagnosis rates reach 1.2 million new cases, highlighting the ongoing expansion of this epidemic ^35.
Racial and Ethnic Disparities
Significant health disparities persist across racial and ethnic groups ^28^35. Among adults with obesity prevalence of 35% or higher, 38 states report this level among Non-Hispanic Black adults, 34 states among Hispanic adults, and 30 states among American Indian or Alaska Native adults ^28. For diabetes, rates are highest among American Indian/Alaska Native adults at 13.6%, followed by Non-Hispanic Black adults at 12.1% and Hispanic adults at 11.7% ^35.
Economic and Healthcare System Implications
Healthcare Cost Burden
The economic implications of the obesity and diabetes epidemics are staggering ^33. Direct medical costs for diabetes increased 35% over the past decade, with people with diabetes accounting for one of every four healthcare dollars spent ^33. The intersection of obesity treatment costs with GLP-1 medication expenses creates complex economic considerations for healthcare systems ^25.
Employer Health Benefits and Coverage Decisions
Corporate health plans show limited coverage of GLP-1 medications, with only 34% providing coverage according to 2024 data ^42. However, employers increasingly recognize potential productivity benefits, including reduced absenteeism, enhanced focus and energy, and improved mental health outcomes ^37. The medications' effects on reducing healthcare utilization for obesity-related complications may provide long-term cost offsets ^37.
Future Implications and Research Directions
Expanding Therapeutic Applications
The comprehensive health benefits demonstrated by GLP-1 medications suggest expanding therapeutic applications beyond diabetes and obesity ^36. Current research investigating addiction treatment, neurodegenerative disease prevention, and kidney disease management may lead to additional FDA approvals ^9^43. The medications' anti-inflammatory effects and impact on multiple organ systems position them as potential treatments for various chronic conditions ^36.
Market Projections and Access Considerations
Analyst projections suggest the GLP-1 market could reach $150 billion by 2030, driven by expanding indications and growing patient populations ^42. However, access challenges related to cost and insurance coverage may limit equitable distribution of these therapies ^19. Policy discussions around Medicare coverage for weight loss indications could significantly impact access for older adults ^19.
Conclusion
GLP-1 receptor agonists represent a paradigm shift in obesity and diabetes treatment, demonstrating unprecedented efficacy across multiple health domains ^1^36. The medications achieve superior weight loss compared to previous interventions while providing cardiovascular protection, addiction reduction benefits, and improvements in sleep apnea and other conditions ^15^17. However, the rapid adoption occurs against a backdrop of worsening obesity and diabetes epidemics, with significant geographic and racial disparities requiring targeted interventions ^28.
The 600% increase in GLP-1 usage from 2019 to 2024 reflects both the medications' effectiveness and the urgent need for obesity treatments ^18. As healthcare systems grapple with the economic implications of both the underlying epidemics and the high cost of treatment, ensuring equitable access while managing fiscal sustainability remains a critical challenge ^25. Future research directions and policy decisions will determine whether these breakthrough therapies can meaningfully impact population health outcomes and reduce the substantial burden of obesity-related diseases ^42.