Fiber is Your Essential Ally on the GLP-1 Weight Loss Journey

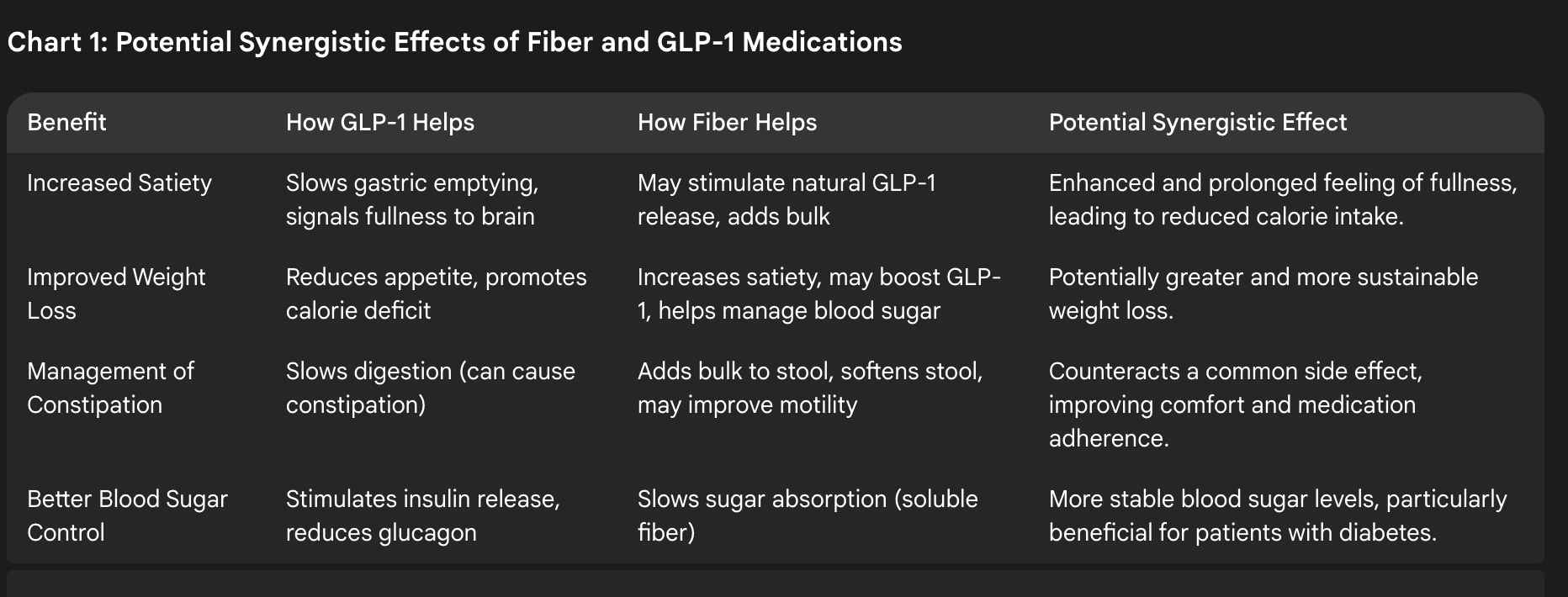
When you begin treatment with GLP-1 medications like Wegovy, Zepbound, Ozempic, or Mounjaro, much of the focus is on what foods to avoid and how to manage side effects. However, there's one nutritional component that deserves special attention: fiber. Understanding how to optimize your fiber intake can dramatically improve your experience with GLP-1 medications and support your overall health transformation.
Why Fiber Matters Even More on GLP-1 Medications
GLP-1 medications slow down digestion and can increase the risk of constipation—a common and uncomfortable side effect that many patients experience. Proper fiber intake is your first line of defense against this issue, but it requires a thoughtful approach. Too little fiber can lead to constipation, while too much all at once might contribute to bloating, especially as your digestive system adjusts to the medication.
Finding the right balance is essential for your comfort and success on this journey.
Understanding Fiber: More Than Just "Roughage"
Fiber is the indigestible part of plants, primarily found in cell walls and structural components. Unlike other nutrients, fiber passes through your digestive system largely intact—we don't have the enzymes to break it down completely. Instead, it works as a digestive passenger with remarkable benefits along the way.
The Fiber Journey Through Your Body
- In your stomach: Fiber absorbs stomach juices and swells, pressing against your stomach walls. This signals fullness to your brain, helping you feel satisfied with less food—a perfect complement to the appetite-suppressing effects of GLP-1 medications.
- In your small intestine: Fiber slows glucose absorption, helping stabilize blood sugar levels—a significant benefit for those using these medications to manage diabetes or insulin resistance.
- In your large intestine: Beneficial gut bacteria feast on fiber, producing compounds that strengthen your immune system and gut health. Additionally, fiber helps bind to cholesterol, preventing its absorption into your bloodstream, which supports heart health.
- On its way out: Fiber adds bulk to waste, helping it move more efficiently through your system, and literally scrubs your intestinal walls, potentially reducing colon cancer risk.
The Two Types of Fiber You Need
Soluble Fiber
Found in: Fruits, root vegetables, oats, barley, legumes (beans and lentils), and soy products
Soluble fiber dissolves in your digestive fluids, forming a gel-like substance that:
- Binds with cholesterol particles, preventing them from entering your bloodstream
- Lowers LDL ("bad") cholesterol levels
- Slows digestion and glucose absorption, helping stabilize blood sugar
- Feeds beneficial gut bacteria
Insoluble Fiber
Found in: Whole grains, wheat bran, nuts, seeds, and the skins of many fruits and vegetables
Insoluble fiber remains largely intact as it travels through your digestive tract:
- Adds bulk to waste material
- Speeds transit time through your intestines
- Acts as nature's internal cleansing system
- Helps prevent constipation and promotes regularity

Finding Your Fiber Sweet Spot on GLP-1 Medications
The Dietary Guidelines for Americans recommend:
- Women: 25 grams per day
- Men: 38 grams per day
- Or approximately 14 grams per 1,000 calories consumed
However, on GLP-1 medications, you might be consuming fewer calories overall, making it challenging to reach these targets. This is where quality becomes even more important than quantity.
The "Start Low, Go Slow" Approach
When increasing your fiber intake while on GLP-1 medications:
- Begin gradually: Adding too much fiber too quickly can cause bloating, gas, and discomfort—especially when your digestive system is already adjusting to medication.
- Increase by small amounts: Add just 2-3 grams of fiber per day each week until you reach your target.
- Drink plenty of water: Fiber needs fluid to work properly. Aim for at least 64 ounces (8 cups) daily, more if you're increasing fiber intake.
- Mix fiber types: Consume a variety of fiber sources to get both soluble and insoluble benefits.
- Monitor your response: Pay attention to how different fiber sources affect you—some may work better for your system than others.
The Bristol Stool Chart: Your Digestive Feedback Tool
One practical way to determine if your fiber intake is appropriate is to monitor your bowel movements using the Bristol Stool Chart:
- Types 1-2: Hard, difficult to pass stools indicate you likely need more fiber and water.
- Types 3-4: Ideal consistency, suggesting your fiber and fluid intake is well-balanced.
- Types 5-7: Loose or watery stools may indicate too much fiber (particularly if you've increased intake rapidly) or other digestive issues.
While it might not be the most glamorous topic, paying attention to these changes provides valuable feedback on how to adjust your fiber intake for optimal digestive health.
Practical Tips for Increasing Fiber on GLP-1 Medications
- Focus on fiber-rich, protein-packed foods: Beans, lentils, edamame, and high-fiber nuts like almonds provide both the protein you need and the fiber that supports digestion.
- Make every bite count: When appetite is reduced, choosing foods that deliver multiple benefits becomes crucial. Opt for berries over lower-fiber fruits, or sweet potatoes with skins over white potatoes.
- Consider fiber supplements when needed: If meeting your fiber needs through food alone is challenging, supplements like psyllium husk can help. Start with a small dose (half the recommended amount) and gradually increase as tolerated.
- Add fiber to foods you're already eating: Sprinkle ground flaxseeds on yogurt, add chia seeds to smoothies, or mix a small amount of wheat bran into your morning oatmeal.
- Create fiber-boosting habits:
- Keep the skins on fruits and vegetables when possible
- Choose whole grain versions of bread, pasta, and cereals
- Snack on high-fiber options like popcorn, raw vegetables, or a small handful of nuts
- Add a tablespoon of beans or lentils to soups, salads, or pasta dishes
When to Be Cautious with Fiber
While fiber is beneficial, there are times when you might need to temporarily reduce intake:
- During severe GLP-1 side effects: If experiencing significant nausea, vomiting, or diarrhea, you may need to temporarily reduce fiber intake until symptoms improve.
- Before medical procedures: Follow your doctor's instructions regarding fiber intake before any digestive system procedures.
- If you have certain digestive conditions: Some conditions may require specialized fiber approaches—consult with your healthcare provider.
The Bottom Line: A Balanced Approach
Fiber is a powerful ally on your GLP-1 journey, helping manage side effects while supporting your long-term health goals. Finding the right balance—not too little, not too much—takes some experimentation, but the benefits to your digestive comfort, heart health, and disease prevention make it well worth the effort.
Remember that your needs may change throughout your treatment. What works during your first month might need adjustment as your body adapts to the medication and as your weight changes. Stay flexible, listen to your body's signals, and partner with your healthcare provider to optimize your approach.
By giving fiber the attention it deserves in your nutrition plan, you're not just managing medication side effects—you're building sustainable habits that will support your health long after you've reached your goals.