The Childhood Obesity Crisis in America: What Parents Need to Know About Treatment Options for Teens

The statistics are sobering: nearly 1 in 5 children and adolescents in the United States struggle with obesity, representing a tripling of rates since the 1970s. For parents watching their teenagers battle weight issues, the emotional and physical toll can be overwhelming. With new medications like Wegovy and Zepbound now approved for adolescents, many families are wondering if these treatments could be the answer they've been searching for.
Understanding the Scope of Childhood Obesity
Childhood obesity has become one of the most pressing public health challenges of our time. According to the Centers for Disease Control and Prevention (CDC), approximately 19.5% of children and adolescents aged 2-19 years have obesity, with rates varying significantly across different demographic groups. Among adolescents aged 12-19, the obesity rate reaches 22.2%, meaning more than one in five teenagers in America is classified as obese.
These aren't just numbers on a chart – they represent millions of young people facing serious health consequences that can follow them into adulthood. Childhood obesity increases the risk of developing type 2 diabetes, high blood pressure, sleep apnea, joint problems, and psychological issues including depression and low self-esteem. Perhaps most concerning is that children with obesity are more likely to become adults with obesity, creating a cycle that can be difficult to break.
The economic burden is equally staggering. The medical costs associated with childhood obesity are estimated to exceed $14 billion annually in the United States. When indirect costs like missed school days and reduced productivity are included, the total economic impact reaches into the tens of billions of dollars each year.
The Complex Web of Causes
Understanding why childhood obesity has reached epidemic proportions requires examining multiple interconnected factors. Unlike adult obesity, which often develops gradually over decades, childhood obesity can emerge rapidly during critical developmental periods, making early intervention crucial.

Dietary Factors
The modern American food environment presents unprecedented challenges for maintaining healthy weight. Ultra-processed foods, which now make up approximately 67% of calories consumed by children and adolescents, are engineered to be hyperpalatable and calorie-dense while being nutritionally poor. These foods are often cheaper and more convenient than whole foods, making them attractive options for busy families.
Portion sizes have grown dramatically over the past several decades. A typical fast-food meal for children today contains nearly twice the calories it did in the 1980s. Sugary beverages, including sodas, sports drinks, and fruit juices, contribute an average of 143 calories per day to children's diets – calories that provide little nutritional value but significantly impact weight gain.
Lifestyle and Environmental Changes
Physical activity levels among children have declined substantially. Many schools have reduced or eliminated physical education programs due to budget constraints and increased focus on standardized testing. The rise of screen time – averaging over 7 hours per day for teenagers – has replaced active play and outdoor activities that previous generations took for granted.
Urban planning and neighborhood design also play crucial roles. Many communities lack safe spaces for children to play outdoors, walkable routes to school, or access to recreational facilities. This "built environment" can make it extremely difficult for families to maintain active lifestyles, regardless of their intentions.
Socioeconomic Disparities
Childhood obesity rates are highest among families with lower incomes and in certain racial and ethnic groups. Hispanic children have an obesity rate of 25.6%, followed by Black children at 24.2%, compared to 16.1% among white children and 8.7% among Asian children. These disparities reflect complex interactions between poverty, food insecurity, limited access to healthy foods and safe places for physical activity, and chronic stress.
Food deserts – areas with limited access to affordable, nutritious foods – disproportionately affect low-income communities and communities of color. Families in these areas may rely on convenience stores and fast-food restaurants for meals, making it challenging to maintain healthy diets even when parents understand the importance of good nutrition.
Psychological and Social Factors
Mental health plays a significant role in childhood obesity. Stress, trauma, depression, and anxiety can all contribute to weight gain through various mechanisms, including emotional eating, disrupted sleep patterns, and reduced motivation for physical activity. The stigma associated with obesity can create additional psychological burden, leading to social isolation and further weight gain.
Family dynamics and parenting styles also influence children's eating behaviors and attitudes toward food. Parents who use food as comfort, reward, or punishment may inadvertently contribute to unhealthy relationships with eating that persist into adulthood.
Health Consequences: More Than Just Numbers on a Scale
The health impacts of childhood obesity extend far beyond cosmetic concerns. Many conditions previously seen only in adults are now appearing in children and teenagers with alarming frequency.
Immediate Health Effects
Type 2 diabetes, once called "adult-onset diabetes," now affects thousands of children and adolescents. Young people with obesity are also at increased risk for high blood pressure, abnormal cholesterol levels, and non-alcoholic fatty liver disease. Sleep apnea, joint problems, and early onset of puberty are additional concerns that can significantly impact quality of life.
Perhaps most troubling are the psychological effects. Children with obesity face higher rates of bullying, social isolation, and discrimination. They're more likely to experience depression, anxiety, and low self-esteem. These mental health challenges can persist into adulthood, affecting educational achievement, career prospects, and relationships.
Long-term Consequences
Children with obesity are approximately five times more likely to have obesity as adults. This increases their lifetime risk of cardiovascular disease, stroke, certain cancers, and premature death. The economic implications are substantial, with individuals who had childhood obesity facing higher healthcare costs throughout their lives.
The reproductive health consequences are also significant. Women who had childhood obesity face increased risks of pregnancy complications, while men may experience fertility issues. The intergenerational nature of obesity means that children of parents with obesity are more likely to develop obesity themselves, perpetuating the cycle.
Traditional Treatment Approaches: Building the Foundation
Before considering medication, healthcare providers typically recommend comprehensive lifestyle interventions that address diet, physical activity, and behavioral factors. These approaches remain the cornerstone of childhood obesity treatment and are essential regardless of whether medications are eventually added to the treatment plan.
Nutritional Interventions
Effective dietary interventions for childhood obesity focus on creating sustainable eating patterns rather than restrictive diets. The goal is to help families develop healthy relationships with food while creating modest caloric deficits that allow for gradual, sustainable weight loss.
Key principles include increasing consumption of fruits, vegetables, whole grains, and lean proteins while reducing intake of processed foods, sugary beverages, and calorie-dense snacks. Portion control education helps families understand appropriate serving sizes, while meal planning and preparation skills ensure that healthy options are readily available.
Many successful programs involve the entire family rather than focusing solely on the child with obesity. This approach recognizes that eating behaviors are learned within the family context and that lasting change requires environmental modifications that support all family members.
Physical Activity Recommendations
Current guidelines recommend that children and adolescents engage in at least 60 minutes of moderate to vigorous physical activity daily. However, for young people with obesity, starting with smaller, achievable goals is often more effective than attempting to meet these recommendations immediately.
Successful physical activity interventions often focus on finding activities that children enjoy rather than forcing participation in traditional sports. Dancing, martial arts, swimming, hiking, or even active video games can provide excellent alternatives for young people who may feel self-conscious about their fitness levels.
Family-based physical activity can be particularly effective. Regular walks, bike rides, or active games create opportunities for bonding while establishing healthy habits. Schools and communities that provide safe, accessible spaces for physical activity play crucial roles in supporting these efforts.
Behavioral and Psychological Support
Behavioral interventions help children and families identify and modify patterns that contribute to weight gain. These might include emotional eating triggers, mindless snacking habits, or using food as entertainment or stress relief.
Cognitive-behavioral therapy (CBT) has shown particular promise in helping young people develop healthier relationships with food and improve body image. Family therapy can address dynamics that may inadvertently support unhealthy behaviors while strengthening family support for lifestyle changes.
Many successful programs also include peer support components, allowing young people to connect with others facing similar challenges. This can reduce feelings of isolation and provide motivation for maintaining healthy behaviors.
The Promise and Complexity of GLP-1 Medications
GLP-1 receptor agonists represent the most significant advancement in obesity treatment in decades. These medications, originally developed for type 2 diabetes, work by mimicking hormones that regulate blood sugar and appetite. In clinical trials, they've demonstrated remarkable effectiveness for weight loss in both adults and adolescents.
How GLP-1 Medications Work
GLP-1 (glucagon-like peptide-1) is a hormone naturally produced in the intestines in response to food intake. It works through multiple mechanisms to regulate glucose levels and food intake, including slowing gastric emptying (making people feel full longer), reducing appetite, and improving insulin sensitivity.
Medications like semaglutide (Wegovy) and tirzepatide (Zepbound) are synthetic versions of GLP-1 that are modified to last longer in the body. They're administered as once-weekly injections and have been shown to produce significant weight loss when combined with lifestyle interventions.
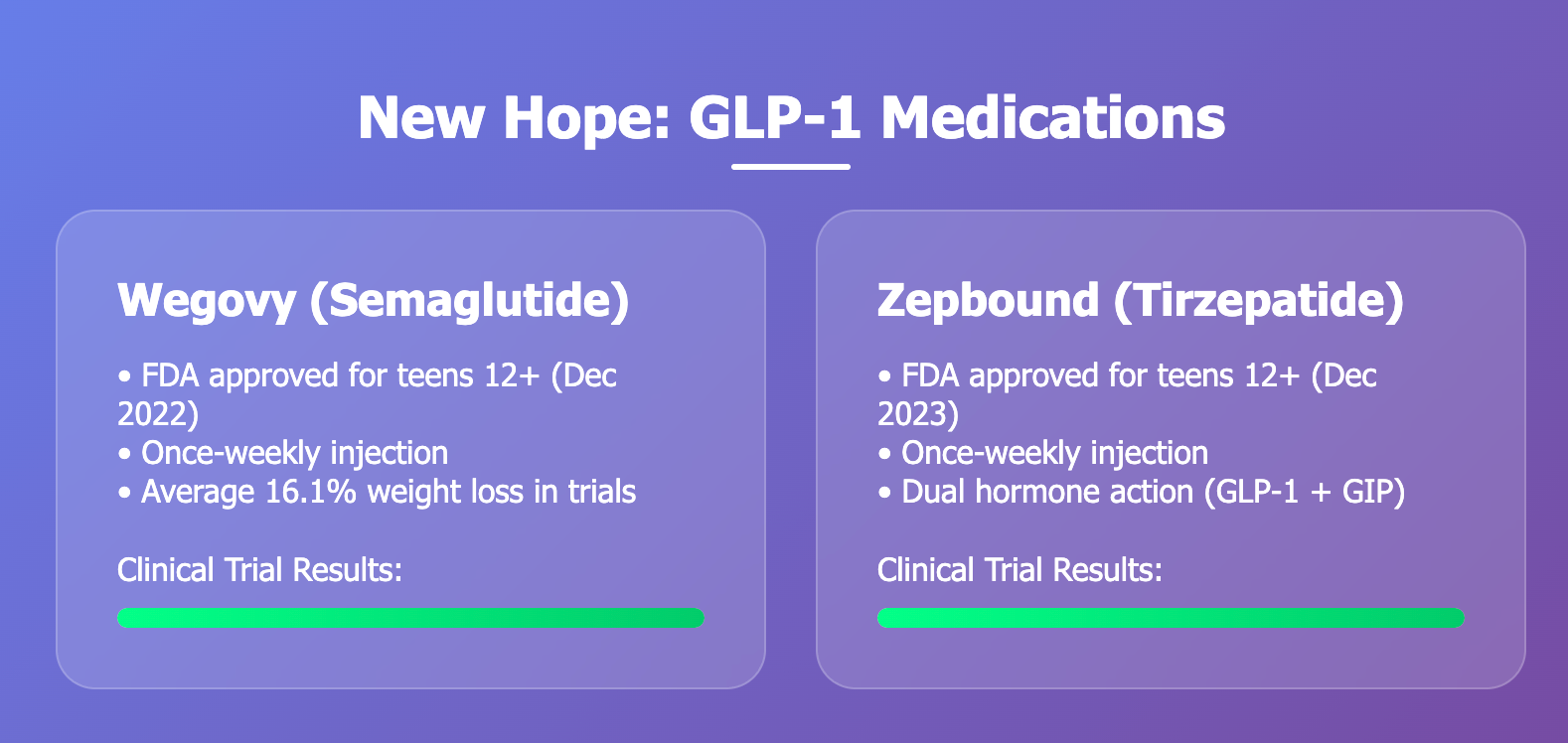
Clinical Evidence in Adolescents
The clinical trial data for GLP-1 medications in adolescents is compelling. In the STEP TEENS study, which evaluated semaglutide in teenagers aged 12-17 with obesity, participants who received the medication along with lifestyle counseling lost an average of 16.1% of their body weight over 68 weeks, compared to just 0.6% in the placebo group.
Similarly impressive results have been seen with tirzepatide, though the pediatric data is more limited. These medications have demonstrated effectiveness across different demographic groups, suggesting they could help address disparities in childhood obesity outcomes.
FDA Approval and Current Guidelines
The FDA approved Wegovy (semaglutide) for adolescents aged 12 and older with obesity in December 2022, making it the first GLP-1 medication approved for this age group. Zepbound (tirzepatide) received approval for adolescents in December 2023. These approvals were based on robust clinical trial data demonstrating both safety and efficacy.
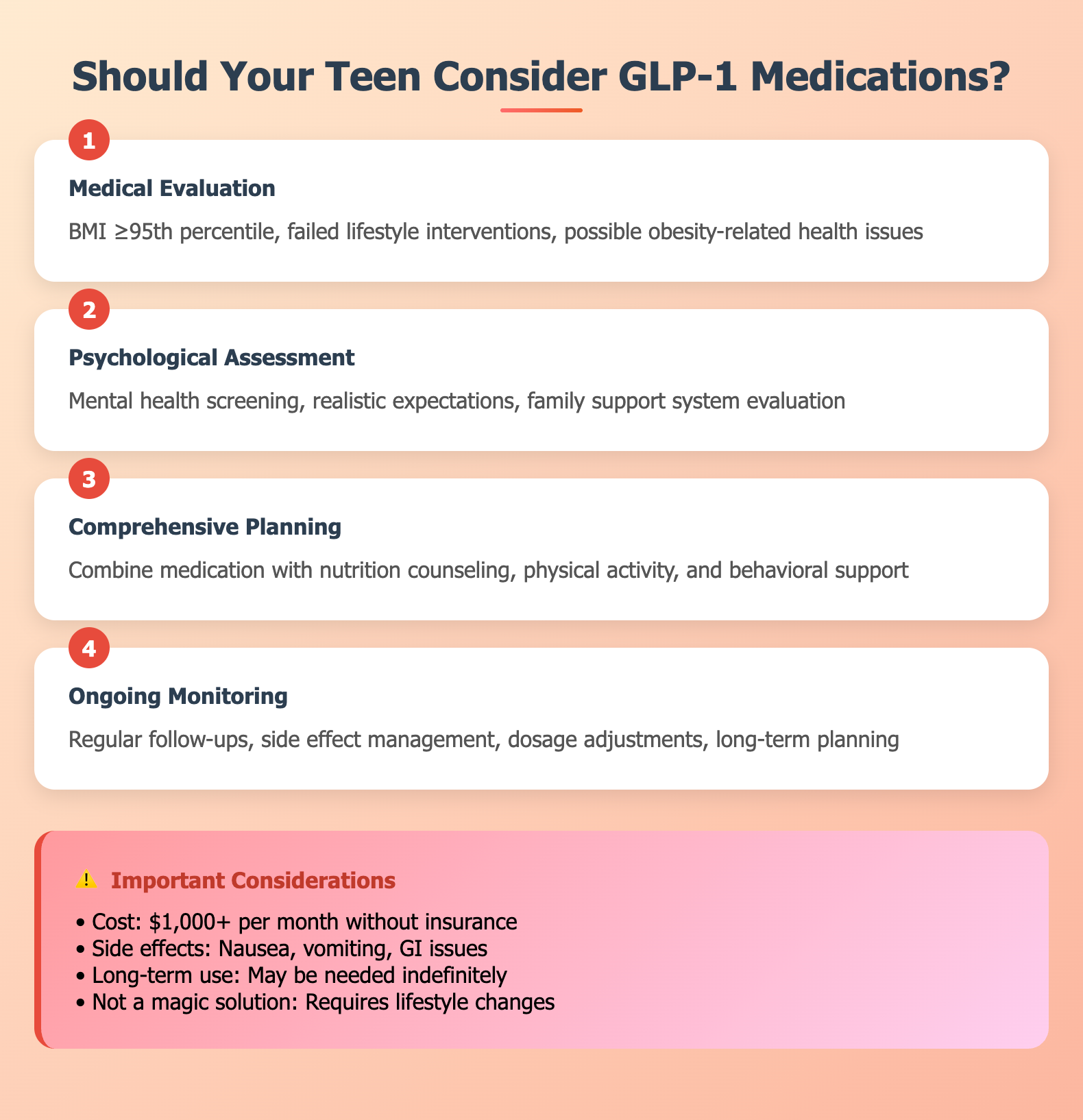
Current guidelines recommend considering these medications for adolescents with a BMI at or above the 95th percentile for age and sex (clinical obesity) who have not achieved adequate weight loss through lifestyle interventions alone. The medications are intended to be used alongside, not instead of, comprehensive lifestyle interventions.
Should Teenagers Take GLP-1 Medications? A Nuanced Answer
The question of whether teenagers should take GLP-1 medications like Wegovy or Zepbound doesn't have a simple yes or no answer. The decision requires careful consideration of multiple factors and should always involve thorough consultation with healthcare providers who specialize in adolescent obesity.
Strong Candidates for GLP-1 Treatment
Teenagers who may be good candidates for GLP-1 medications typically have several characteristics. They have clinical obesity (BMI ≥95th percentile) that has persisted despite sustained efforts with lifestyle interventions. They may have obesity-related health complications such as type 2 diabetes, high blood pressure, or sleep apnea that require urgent intervention.
These adolescents often have strong family support systems that can help ensure medication adherence and continued lifestyle modifications. They understand that the medication is a tool to be used alongside, not instead of, healthy eating and physical activity. Many have worked with healthcare providers, dietitians, or other specialists and have demonstrated commitment to making lifestyle changes.
Psychological readiness is also important. Teenagers who are good candidates typically have realistic expectations about the medication's effects and understand that weight loss will be gradual. They're prepared for potential side effects and have support systems to help them navigate any challenges that arise.
Situations Requiring Caution
Several factors might make GLP-1 medications less appropriate for certain teenagers. Very young adolescents (ages 12-13) may require more careful consideration, as the long-term effects of these medications in this age group are still being studied. Teenagers with certain medical conditions, including a personal or family history of thyroid cancer or multiple endocrine neoplasia syndrome, may not be suitable candidates.
Mental health considerations are crucial. Adolescents with active eating disorders, severe depression, or other psychiatric conditions may need these issues addressed before starting weight-loss medications. The psychological impact of rapid weight loss can be significant, particularly for teenagers who are still developing their sense of identity.
Family dynamics also matter. Teenagers whose families are not supportive of lifestyle changes or who may face criticism or unrealistic expectations about weight loss may not be good candidates for medication treatment. The cost and insurance coverage issues can also create barriers for many families.
The Importance of Comprehensive Care
When GLP-1 medications are appropriate, they should always be part of a comprehensive treatment plan that includes nutritional counseling, physical activity recommendations, behavioral support, and regular medical monitoring. The most successful outcomes occur when medications are used as tools to help teenagers make lifestyle changes more effectively, not as standalone solutions.
Regular follow-up appointments are essential to monitor effectiveness, adjust dosing, manage side effects, and provide ongoing support. Many teenagers benefit from working with multidisciplinary teams that include pediatric endocrinologists or obesity medicine specialists, registered dietitians, mental health professionals, and other specialists as needed.
Considerations and Potential Challenges
While GLP-1 medications offer significant promise, they also present unique challenges when used in adolescents that families and healthcare providers must carefully consider.
Side Effects and Safety Concerns
The most common side effects of GLP-1 medications are gastrointestinal, including nausea, vomiting, diarrhea, and constipation. These effects are usually mild to moderate and often improve over time, but they can be particularly challenging for teenagers who may already feel self-conscious about their bodies or eating habits.
More serious but rare side effects include pancreatitis, gallbladder problems, and kidney issues. There have been concerns about thyroid tumors based on animal studies, though this risk hasn't been confirmed in humans. Regular monitoring and open communication between teenagers, families, and healthcare providers are essential for identifying and managing any adverse effects.
The psychological side effects deserve special attention in adolescents. Some young people experience mood changes, and there have been reports of suicidal ideation in some patients taking these medications, though a causal relationship hasn't been established. Given that adolescence is already a time of significant emotional and psychological development, careful monitoring of mental health is crucial.
Cost and Access Issues
The cost of GLP-1 medications can be substantial, with monthly prices often exceeding $1,000 without insurance coverage. While many insurance plans now cover these medications for adults with obesity, coverage for adolescents is less consistent and may require prior authorization or documented failure of other treatments.
This creates significant equity concerns, as families with higher incomes may have better access to these potentially life-changing treatments. Some pharmaceutical companies offer patient assistance programs, but navigating these programs can be complex and time-consuming.
Long-term Considerations
One of the most significant unknowns about GLP-1 medications in adolescents is what happens when treatment stops. In adult studies, most people regain a significant portion of lost weight when they discontinue the medication. This raises important questions about the duration of treatment and the need for long-term medication use.
For teenagers, who may potentially need decades of treatment, the long-term safety and cost implications are substantial. There's also the question of how these medications might affect normal adolescent development, though current evidence suggests they don't interfere with growth or sexual maturation.
Making the Decision: A Family-Centered Approach
The decision about whether a teenager should use GLP-1 medications requires careful consideration of the individual adolescent's medical, psychological, and social circumstances. This decision-making process should involve the teenager, their parents or guardians, and qualified healthcare providers.
Working with Healthcare Providers
Families considering GLP-1 medications for their teenagers should seek care from providers with expertise in adolescent obesity. This might include pediatric endocrinologists, adolescent medicine specialists, or physicians certified in obesity medicine. These specialists can provide comprehensive evaluations and ongoing monitoring that general pediatricians may not be equipped to offer.
The evaluation process typically includes detailed medical and psychological assessments, review of previous weight loss attempts, assessment of family support systems, and discussion of realistic expectations and potential risks. Providers should also assess the teenager's readiness to make lifestyle changes and their understanding of the medication's role in their overall treatment plan.
Supporting Teenagers Through Treatment
Teenagers who start GLP-1 medications need ongoing support to maximize their chances of success. This includes regular medical monitoring, nutritional counseling, and psychological support as needed. Families play crucial roles in creating supportive environments that encourage healthy behaviors while avoiding excessive focus on weight or appearance.
School support may also be important, particularly if teenagers experience side effects that affect their daily activities or if they need accommodations for medical appointments or dietary needs. Open communication between families, healthcare providers, and schools can help ensure that teenagers receive comprehensive support.
The Broader Context: Prevention and Public Health
While GLP-1 medications offer hope for individual teenagers struggling with obesity, addressing the childhood obesity epidemic requires broader public health approaches that focus on prevention and creating environments that support healthy behaviors for all children.
Community and Policy Solutions
Effective prevention strategies require changes at multiple levels, from individual families to national policies. Schools can play crucial roles by providing nutritious meals, ensuring adequate physical education, and creating environments that promote healthy behaviors. Communities can invest in safe spaces for physical activity, improve access to healthy foods, and implement policies that support active transportation.
Healthcare systems need to prioritize obesity prevention and early intervention, providing families with resources and support before obesity develops. This includes training more healthcare providers in obesity medicine and ensuring that preventive services are accessible to all families regardless of income or insurance status.
The Role of Technology and Innovation
Technology offers promising tools for supporting both prevention and treatment of childhood obesity. Mobile apps, wearable devices, and telehealth platforms can provide personalized support, track progress, and connect families with resources and support networks. However, these tools must be designed thoughtfully to avoid creating additional stress or unhealthy behaviors.
Virtual reality and gaming technologies are being explored as ways to make physical activity more engaging for young people who might otherwise be sedentary. These innovations could be particularly valuable for reaching adolescents who feel self-conscious about traditional forms of exercise.
Looking Forward: Hope and Responsibility
The availability of effective medications like Wegovy and Zepbound represents a significant advancement in treating adolescent obesity, offering hope to families who have struggled with traditional approaches. However, these medications are not magic bullets that eliminate the need for lifestyle changes or address the underlying factors that contribute to the obesity epidemic.
For individual teenagers, the decision to use GLP-1 medications should be made carefully, with thorough consideration of the potential benefits and risks, strong medical supervision, and commitment to comprehensive lifestyle interventions. These medications can be powerful tools for helping motivated teenagers achieve healthier weights and reduce obesity-related health risks.
At the same time, we must not lose sight of the need for broader societal changes that address the root causes of childhood obesity. Creating environments where all children can easily access healthy foods and opportunities for physical activity, addressing socioeconomic disparities that contribute to obesity, and supporting families in making healthy choices are essential for preventing obesity in future generations.
The childhood obesity epidemic didn't develop overnight, and it won't be solved by any single intervention. However, the combination of effective individual treatments like GLP-1 medications for those who need them, comprehensive lifestyle interventions for all children with obesity, and broader prevention efforts offers genuine hope for creating a healthier future for America's children.
Parents facing decisions about their teenagers' health should work closely with qualified healthcare providers, seek support from other families in similar situations, and remember that addressing childhood obesity is a journey that requires patience, persistence, and compassion. With the right combination of medical care, family support, and societal changes, we can help more young people achieve healthier, happier lives.